If you are interested in a proven new revenue stream while at the same time being able to provide access to courses that will lift up your providers and staff, we’d love to speak with you. We’d love to explain how a training partnership with Practice Management Institute can positively affect not only your bottom line, but enhance your role as a steward of the success of the providers and practices you serve. Here’s a testimonial from one of your peers:
“The Medical Society of Delaware is delighted to underscore the exceptional value and numerous benefits that our educational partnership has brought to our esteemed members and their medical practices. Since the inception of this collaboration, we have witnessed transformative outcomes that have significantly contributed to their professional growth and success.
Read More
Topics:
medical billing,
medical coding,
patient billing,
medical office training,
physician relations
-1.png)
Practice Management Institute Partners with Hendrick Health Regional Services to Bring Important Web-based Programming to 139 Affiliated Regional Practice Staff
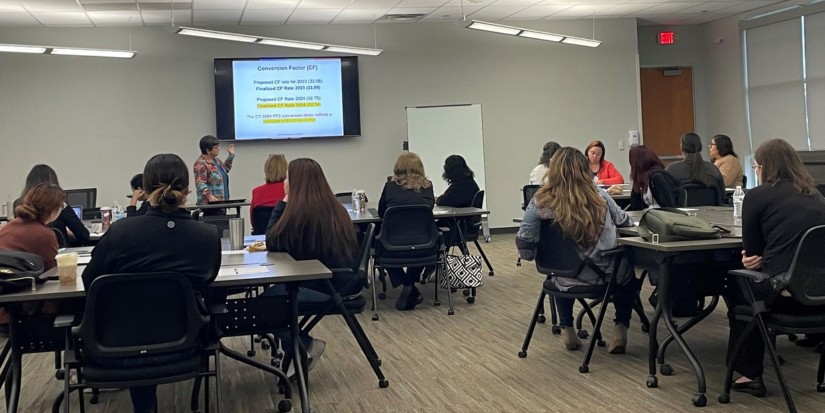
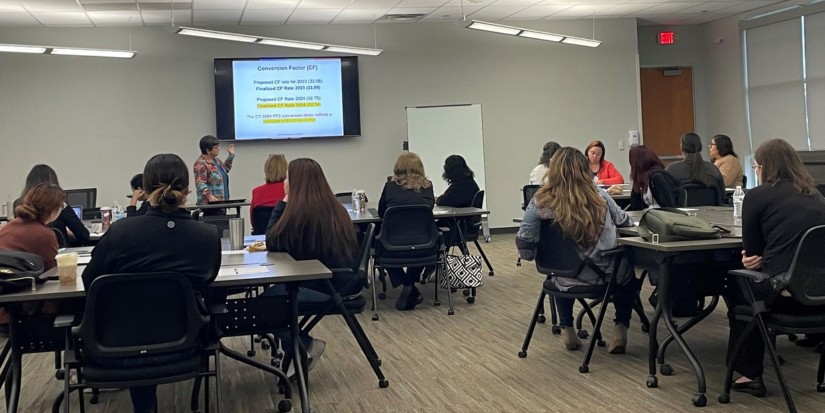
On 2/9/2024 , Hendrick Health Regional Services will host the important Patient Collections/Accounts Receivable Management and E/M Chart Auditing for Physician Services 3-hour webinars to affiliated practice staff in Abilene and 19 West-Texas Counties.
The Patient Collections/Accounts Receivable Management course covers A/R as well as compliance and practice management efforts. Students will learn to improve insurance data collection, eligibility verification, patient communication, and to reduce payment problems that can crush the bottom-line success of the practice. In our E/M Chart Auditing for Physician Services session, participants will learn to improve knowledge of level of service audits to reduce practice risk /promote accurate claim submission. The sessions will be led by PMI faculty leader Jan Hailey MHL, CMC, CMCO, CMIS, CMOM, CMCA E/M, and moderated by Jessica Yourdon, PMI’s Social Media & Content Coordinator.
Sincere thanks to Craig Hunnicutt, Director, Regional Services, Kim Hudson, Coordinator of Provider Outreach and to Amanda Goodson, Provider Outreach, for the consistently demonstrated commitment they each have to the success of medical practices, providers, and staff served regionally by Hendrick Health. What a turnout!
Interested in a similar academic partnership with PMI? If your organization would like more information about partnering with PMI, please contact Michael Moore at 800-259-5562, Ext. 270 or email Michael directly at mmoore@pmimd.com.
Read More
Topics:
medical billing,
medical coding,
patient billing,
medical office training,
physician relations
Practice Management Institute Expands Partnership with Tyler Junior College to Bring Important Continuing Education Opportunities to Local and Regional Medical Practice Staff
PMI is pleased to announce that we are expanding our partnership with Tyler Junior College (TJC). Working closely to offer PMI continuing educational programming covering front desk operations, patient experience, coding, billing, compliance, and reimbursement, as well as the nationally recognized PMI certifications, this new phase in our partnership will focus exclusively on the success of the local and regional healthcare industry, providers, and practice staff.
Read More
Topics:
medical billing,
medical coding,
patient billing,
medical office training,
physician relations
Practice Management Institute (PMI) has named Washington County Community College (WCCC) its 2023 Outstanding National Host Partner. The award, chosen nationally from among hundreds of hospital, college, medical society, physician service group and program host partners, is given to an organization who has demonstrated exceptional commitment to partnering with PMI for the purposes of advancing educational opportunities within their service area and state.
Read More
Topics:
medical billing,
medical coding,
patient billing,
medical office training,
physician relations

This week in Buffalo- PMI will present new instructor-led webinars with long-time PMI host Catholic Medical Partners.
PMI is a proud educational partner of Catholic Medical Partners in Buffalo, NY. For 27 years, we have joined forces to provide quality educational and credentialing programming to local and regional medical practice staff, and we’re thrilled to kick off yet another year of much needed programming to keep practice staff in the know.
Leading the 2024 Reimbursement Update: CPT© and Medicare Compliance and Mastering EM Coding sessions will be PMI faculty presenter Audrey Coaxum, CHC, CPC, CEMC, CMC, CMIS, CMOM, CMCO. Audrey is an exceptional instructor, and is known nationally for her easy to follow teaching skills and exceptional knowledge base.
New CPT® code and regulatory changes for 2024 will go into effect on January 1st. Numerous proposals include conversion factor payment increases for primary care / direct patient care, caregiver training services, and services involving community health workers, care navigators, and peer support specialists. The implementation of a separate add-on payment for HCPCS code G2211 is also proposed, which is expected to improve the accuracy of payment for primary and longitudinal care.
In the morning session, Audrey will help prepare attendees for the impact of coding and regulatory changes. This annual update program will help students forecast the impact on billing for their particular specialty in 2024. The training will help participants reduce denials and stay in compliance in the New Year. All proposed key changes to the procedural code set, guidelines and issues that may impact provider reimbursement are being addressed.
E/M lays the groundwork for the reimbursement process. It is also a well-known audit trigger. In the afternoon Mastering EM Coding session, Audrey will provide the tools needed to internally monitor billing compliance. Participants will learn to relate accurate code selection to proper reimbursement, and will receive a comprehensive explanation of E/M coding and documentation guidelines, and identification of accurate and clinically useful information.
Huge shout out to Lea Passage, MHA, CLP, Physician’s Relations Specialist, for once again playing host, and for continually having the backs of her providers and staff.
The Catholic Medical Partners mission is to provide a high-performing health care system that continuously improves upon the delivery of health care to the populations they service, and to demonstrate improvements in the patient experience, preventative health, and the care and treatment of patients with high burden of illness with a lower the cost trend.
Read More
Topics:
medical billing,
medical coding,
patient billing,
medical office training,
physician relations
PMI is a proud educational partner for University Health in San Antonio. This stellar organization is growing in San Antonio with a powerful, positive impact on the community. We congratulate them on the new Women’s and Children’s Hospital, and could not be more grateful for the partnership, which brings regularly scheduled, high-quality training and credentialing programs to regional practice staff.
Today, PMI faculty/presenter Lisa Maciejewski-West, CMC, CMIS, CMOM, CMCA-E/M, CPCO, owner of Gold Star Medical Business Services, taught morning and afternoon sessions: 2024 Reimbursement Update: CPT and Medicare Compliance. Lisa teaches with a great deal of experience and know-how, and her uplifting and engaging presentation style makes for a great session. So well done!
New CPT® code and regulatory changes for 2024 will go into effect on January 1st. Numerous proposals include conversion factor payment increases for primary care / direct patient care, caregiver training services, and services involving community health workers, care navigators, and peer support specialists. The implementation of a separate add-on payment for HCPCS code G2211 is also proposed, which is expected to improve the accuracy of payment for primary and longitudinal care.
Lisa is helping to prepare attendees for the impact of coding and regulatory changes. This annual update program will help students forecast the impact on billing for their particular specialty in 2024. The training will help participants reduce denials and stay in compliance in the New Year. All proposed key changes to the procedural code set, guidelines, and issues that may impact provider reimbursement are being addressed.
We’d like to thank Magdalena Barrera, University Health Assistant Director of Outreach and Business Development, for hosting another successful day of training. Magdalena is as good as it gets in a host-partner liaison.
Read More
Topics:
medical billing,
medicare,
medical coding,
medicare compliance,
patient billing,
medical office training,
Client Relations
When a Medicare patient has multiple sources of insurance coverage, Medicare will only pay for services after the primary payer has processed the claim and made their payment. Medical office staff must always verify the patient's insurance coverage thoroughly - gathering all necessary information from the primary insurance, such as policy numbers, claim submission instructions, and any preauthorization requirements, etc.
Read More
Topics:
Practice cash flow,
payer contract,
carrier contract,
carrier contract guidelines,
medicare compliance,
patient billing,
claims,
insurance
Pain management treatments are primarily performed by an interventional pain management specialist, physiatrist, anesthesiologist, orthopedic surgeon, or neurosurgeon, and can include physical or occupational therapy, over-the-counter or prescription medication, neurostimulators, and injections.
Read More
Topics:
medical billing,
Pain Management,
medical coding,
patient billing,
medical office training
Consumer healthcare spending continues to rise, not surprisingly due in part to the COVID-19 pandemic. National health spending projections for 2021-23 will continue to inch upward 5.4 percent per year, according to research compiled by the National Health Expenditures Accounts (NHE). Insurers have tightened the reins shifting more financial burden to their members. And with inflation, furloughs, unpaid family leave, and mounting medical and prescription costs, it's no surprise that family budgets are stretched thin.
Read More
Topics:
Practice debt,
medical practice issues,
medical billing,
patient billing,
patient collections
If you work with provider claims in a medical office, then you have probably heard the phrase, “If it isn’t documented, it wasn’t done.” But a 2020 Center for Medicare and Medicaid Services (CMS) report found that more than 70 percent of claims submitted for payment were paid improperly, meaning something was incomplete or missing from the documentation submitted with a claim.
Read More
Topics:
carrier contract guidelines,
medical billing,
Medicare fraud,
medicare compliance,
patient billing
How would you characterize the success of your medical office? Is it a steady flow of patients, low denials, providers that take an active role in the business, a great clinical and administrative team? How about the financial health of the practice? It’s hard to guide the ship in the right direction when you are too busy plugging holes in the galley.
Read More
Topics:
Practice management,
Practice cash flow,
medical practice issues,
financial management,
patient billing,
patient collections

%20(3)-1.png)
-1.png)