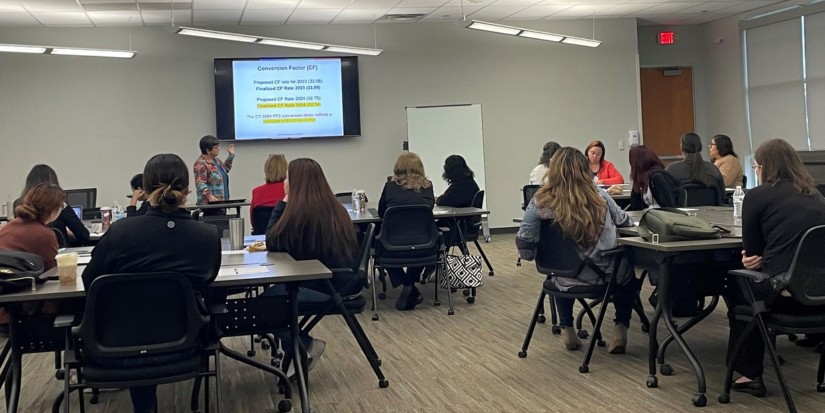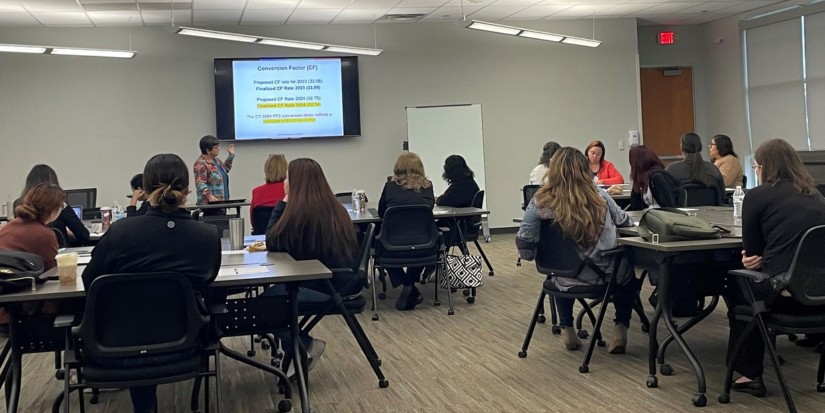
PMI is a proud educational partner for University Health in San Antonio. This stellar organization is growing in San Antonio with a powerful, positive impact on the community. We congratulate them on the new Women’s and Children’s Hospital, and could not be more grateful for the partnership, which brings regularly scheduled, high-quality training and credentialing programs to regional practice staff.
Today, PMI faculty/presenter Lisa Maciejewski-West, CMC, CMIS, CMOM, CMCA-E/M, CPCO, owner of Gold Star Medical Business Services, taught morning and afternoon sessions: 2024 Reimbursement Update: CPT and Medicare Compliance. Lisa teaches with a great deal of experience and know-how, and her uplifting and engaging presentation style makes for a great session. So well done!
New CPT® code and regulatory changes for 2024 will go into effect on January 1st. Numerous proposals include conversion factor payment increases for primary care / direct patient care, caregiver training services, and services involving community health workers, care navigators, and peer support specialists. The implementation of a separate add-on payment for HCPCS code G2211 is also proposed, which is expected to improve the accuracy of payment for primary and longitudinal care.
Lisa is helping to prepare attendees for the impact of coding and regulatory changes. This annual update program will help students forecast the impact on billing for their particular specialty in 2024. The training will help participants reduce denials and stay in compliance in the New Year. All proposed key changes to the procedural code set, guidelines, and issues that may impact provider reimbursement are being addressed.
We’d like to thank Magdalena Barrera, University Health Assistant Director of Outreach and Business Development, for hosting another successful day of training. Magdalena is as good as it gets in a host-partner liaison.
Read More
Topics:
medical billing,
medicare,
medical coding,
medicare compliance,
patient billing,
medical office training,
Client Relations
When a Medicare patient has multiple sources of insurance coverage, Medicare will only pay for services after the primary payer has processed the claim and made their payment. Medical office staff must always verify the patient's insurance coverage thoroughly - gathering all necessary information from the primary insurance, such as policy numbers, claim submission instructions, and any preauthorization requirements, etc.
Read More
Topics:
Practice cash flow,
payer contract,
carrier contract,
carrier contract guidelines,
medicare compliance,
patient billing,
claims,
insurance
Whether you are new to Practice Management Institute, a certified professional, enrolled in, or inquired about medical office training, you have probably interacted with Kathleen Riexinger at some point. She has worked with PMI for two decades and recently received a well-deserved promotion to Director of Student Experience. She chose the new title, said PMI President/CEO David T. Womack, and it fits her to a tee.
Read More
Topics:
Practice management,
medical office manager topics,
medical practice issues,
medical office staff,
administrative burdens,
medical office leadership,
medicare compliance
If you work with provider claims in a medical office, then you have probably heard the phrase, “If it isn’t documented, it wasn’t done.” But a 2020 Center for Medicare and Medicaid Services (CMS) report found that more than 70 percent of claims submitted for payment were paid improperly, meaning something was incomplete or missing from the documentation submitted with a claim.
Read More
Topics:
carrier contract guidelines,
medical billing,
Medicare fraud,
medicare compliance,
patient billing
The U.S. Department of Justice (DOJ) on May 26 announced law enforcement actions for several COVID-19-related Medicare fraud schemes totaling $143 million. The actions involved the exploitation of Centers for Medicare and Medicaid Services (CMS) policies designed to increase access to care during the COVID-19 pandemic. Fourteen defendants were charged for their actions involving the exploitation of the broadened COVID-19 emergency declaration, telehealth regulations, and rules.
Read More
Topics:
medical office compliance,
medical fraud,
Medicare fraud,
medicare compliance